By Matthew Barakat, Associated Press
FALLS CHURCH, Va. — Some people call them floaters. Eye doctors call them “vitreous opacities.” Emily Flynn of Dunedin, New Zealand, called hers “a little fuzzball.” She flew halfway around the world to have it removed.
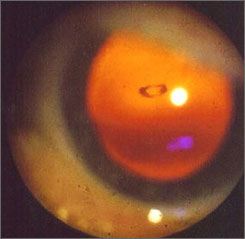
After more than 100 pinpoint zaps from a laser beam during a half-hour visit to a northern Virginia office park, the fuzzball was gone, obliterated within the clear, gelatinous goo that fills the eyeball.
The surgeon, John Karickhoff, has done the same procedure more than 1,400 times over the past 15 years and claims a success rate of better than 90%, with minimal risk of complications. Still, many ophthalmologists have never heard of the procedure — and most would recommend against it. The procedure has drawn regulatory scrutiny in Florida.
Nearly everybody has floaters or will develop them at some point in life, especially older and nearsighted people. Sometimes shaped like specks or snakes, they float through a person’s field of vision, and are most easily seen when you look against a light background like a blue sky or a white wall.
They are harmless, usually just bits of membrane that have become dislodged from other parts of the eye. Karickhoff estimated that 95% of people who have floaters ought to leave them alone. But for that 5%, they can be a legitimate problem.
“I’ve had musicians who couldn’t read the sheet music quickly enough because the floater would get in the way,” said Karickhoff, who has tried for years to get the procedure accepted into the medical mainstream. “It can ruin a patient’s quality of life.”
Only a handful of doctors in the United States — perhaps as few as two — regularly treat floaters with laser surgery.
“Patients usually are told to learn to live with it,” Karickhoff said. “By the time they come to see me, they’ve already seen two or three other doctors.”
Richard Bensinger, a spokesman for the American Academy of Ophthalmology, said most ophthalmologists believe the procedure is unnecessary. He acknowledged the laser treatment is often successful and carries little risk, but most doctors believe any risk is unacceptable for treating a benign condition like floaters.
If patients insist on treatment, Bensinger said the laser treatment can be a better choice than the more common alternative, a vitrectomy, which involves removing most or all of the eyeball’s internal fluid.
The vast majority of patients can learn to live with floaters, Bensinger said. Those patients who demand treatment, he said, “are mostly obsessive-compulsive types” who allow the floaters to drive them to distraction.
But Oliver Hill, 60, of Waynesburg, Pa., said many eye doctors are too dismissive of how irritating a floater can be. He compared it to trying to read a book while holding a pencil directly in front of one of your eyes.
“It just drove me right up the wall,” said Hill, who had his left eye treated in June 2005 and returned to Karickhoff in November to treat a floater in his right eye.
In Flynn’s case, her optometrist in New Zealand had told her that floaters were common and not harmful, and that she should learn to live with it. She learned about Karickhoff from his website.
Before having the surgery, Flynn said she would get headaches as she read and often tried to read with one eye shut to keep the floater out of her line of sight.
“That eye was effectively dysfunctional,” Flynn said.
Karickhoff said he knows firsthand that floaters can be troubling — he had what he called “a whopper” of a floater in his own eye.
He was skeptical when, on a Florida vacation, he saw a newspaper ad touting laser surgery for floaters. But he sat in on a surgery performed by Fort Myers ophthalmologist Scott Geller and later allowed Geller to operate on his eye. The procedure was a success.
Not long after, Karickhoff began performing the procedure himself. Both Geller and Karickhoff have since operated on thousands of patients.
Last year, the Florida Board of Medicine investigated a complaint against Geller filed by a 72-year-old woman who complained that the surgery merely broke up one large floater into a bunch of smaller floaters. But the board dismissed the complaint after hearing testimony from Karickhoff on how the procedure works.
Karickhoff, who has a clean record with the Virginia medical board, said he can tell by examining the patient’s eye if the floater is a serious distraction or a minor annoyance. He declines to treat those “who are making a mountain out of a mole hill” because such patients will almost never be satisfied.
There is little peer-reviewed literature about the procedure. What does exist shows the procedure to be generally safe, but the results about its effectiveness are mixed.
Karickhoff said studies have not replicated his success rate because they have not fully emulated his technique, which requires a laser beam of a specific intensity, and because they have not always chosen ideal candidates for surgery.
Karickhoff said there is a theoretical risk of serious complications, including a detached retina, but that he has never seen it happen. He said his own rate of complications is about a tenth of a percent, usually involving increased pressure within the eye.
Geller likened laser treatment of floaters to “an orphaned surgical procedure” that has been unable to overcome entrenched skepticism.
Despite that skepticism, Karickhoff said the medical community has not been completely unresponsive. He has written a medical book about the procedure, and said he received mostly positive feedback when he presented his work in November at the national conference of the American Academy of Ophthalmology. And insurers frequently cover the procedure, he said.
Manfred von Fricken, chief of ophthalmology at Inova Fairfax Hospital,said he has seen many of Karickhoff’s patients who have benefited from the surgery.
“It’s an innovative approach,” said von Fricken, who agrees that eye doctors are too often dismissive of patient complaints about floaters. “He’s thinking out of the box, and I think it’s pretty imaginative.”
Copyright 2007 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.
http://usatoday30.usatoday.com/news/health/2007-01-27-floaters_x.htm?csp=34